Maxillofacial Trauma– Dr Anna Fang
- Associated complications- airway compromise, hemorrhage, C spine injury, TBI, ocular injury, nerve injury
- Orbital injuries
- CANNOT MISS: ruptured globe, retrobulbar hematoma, entrapment
- Exam: pupils, EOM, pressures, visual acuity, +/- fluorescein
- Stretch of optic nerve can lead to oculo-cardiac reflex- brady, nausea, syncope
- Orbital fractures
- Fractures of the wall can lead to entrapment or hematoma
- Limited EOM in the setting of trauma can be indicator of occult fracture
- Isolated fracture with normal exam can be DC with close follow up
- Ophtho consult: abnormal physical exam, entrapment, globe rupture, laceration
- Typically should have a maxillofacial consult if available
- Zygomatic injuries
- Makes up the walls of the orbit and maxillary sinus
- Exam: can appreciate depression inferiorly and laterally to the eye
- Non-displaced fractures can be discharged with sinus precautions
- Complex fractures need maxillofacial consult +/- ophtho
- Antibiotics for open fractures (typically unasyn)
- Nasal injuries
- CANNOT MISS: nasal septal hematoma, CSF leak
- Exam: be sure to inspect the inferior aspect of the nares
- Closed fractures without swelling can be discharged with delayed follow-up
- Early fracture reduction does not have better outcomes
- Complicated fractures should be seen by ENT/max face
- Look for external and internal lacerations
- Open treated with antibiotics
- Septal hematomas
- Will have hematoma that forms along the septum of the nares
- Drainage: topical lidocaine and vasoconstrictors, aspirate or incise with 15 blade, nasal packing after
- Midface/Maxillary fractures
- Made up of the maxilla, orbit, and the zygoma
- Assess bite for all maxillary/mandibular fractures
- Le Fort fractures associated with other injuries and high injury mechanism
- Type 1: separation of the maxilla
- Type 2: separation of the maxilla and nasal bone
- Type 3: floating face involving the maxilla, orbit, zygoma, and nasal bone
- High risk for surgical airway
- Will all need maxillofacial consult
- Mandibular injuries
- Commonly fractures in two locations
- Exam: tongue depressor test (bilateral), intraoral exam to look for lacerations
- Intraoral lacerations > open fracture
- Consult for open fractures and start antibiotics
- Closed fractures can be discharged with outpatient follow up
- Pressure dressing along the jaw/scalp to stabilize the jaw
- Dental injuries
- Urgent consult for avulsion, intrusion (>3mm), ellis 3 tooth fracture (fracture through the enamel, dentin, and pulp)
- Where did the teeth go??? CXR or CT for evaluation
- Management
- In severe maxillofacial trauma there is a high likelihood of a need for a surgical airway
- Can be very difficult to bag these patients, be cautious using nasal airway adjuncts, reassess frequently
- Bleeding in facial trauma
- Pack the bleeding cavities (oral and nasal), IR late for embolization
- In severe maxillofacial trauma there is a high likelihood of a need for a surgical airway
- Exam considerations
- Full facial nerve (motor and sensory), rock the hard palate, assess for bite, full ocular examination, evaluate inner ear and oral cavity
- Social Determinants
- Have a high suspicion for domestic violence as a potential etiology and NAT in children
- Resources
- Facial trauma management resource
- LITFL summary of facial trauma
Hemorrhage in Pediatric Trauma– Dr Chisom Nnadi
- Leading reversible cause of death in pediatric patients
- In massive hemorrhage hypoxia, acidosis, and hypothermia can lead to coagulopathy complicating resuscitation
- After receiving 2-4u pRBC patients can have hypocalcemia due to chelation factors in blood
- First stop the bleeding (pressure, proximal compression, hemostatic agents, elevation, splinting)
- Hard signs of arterial bleed: expanding, pulsatile, thrill/bruit, loss of distal pulses
- Indications for ED thoracotomy: presence of spontaneous circulation in the field OR hemodynamic instability in trauma AND presence of trauma/thoracic surgeon
- Contraindications similar to adults (no signs of life, asystole, etc.)
- Remember that pediatrics patients can compensate more than adults and will often present tachycardic when in shock but no hypotensive
- Lab testing: type and screen, lactate, CBC, PT/INR, PTT, fibrinogen, electrolytes
- Pediatric patients will become hypothermic more easily than adults, so may want to use rapid transfuser to warm
- Volume of blood products
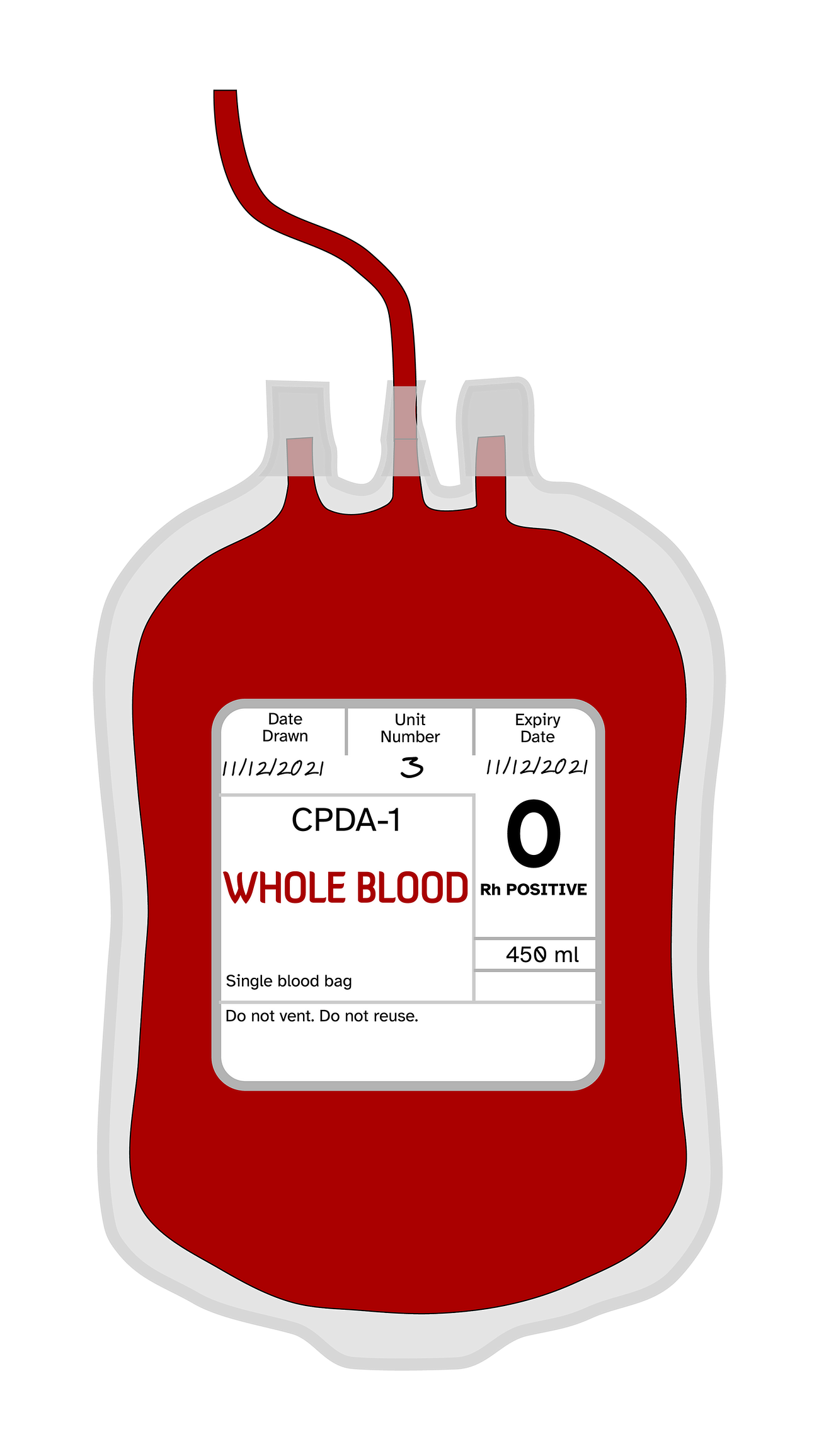
- pRBC are 250-300cc/unit, whole blood is 450cc/unit
- pRBC dosing 10cc/kg
- At BMC no whole blood for patients under 50kg
- Use uncrossmatched O-
- TXA is recommended in pediatric patients
- Goal is permissive hypotension
- Resources
- EMRAP Pediatric major trauma
- EMDocs: Pediatric trauma pearls and pitfalls
- EAST Guidelines for pediatric EDT
Chest Pain in Pregnancy– Dr Alexandra Van Besien
- PE most common in the 3rd trimester, 4x higher risk after C-section
- No validated criteria in pregnant patient for ruling out PE
- Keep in mind there is not external validation for YEARS
- Multiple recommendations against the use of DDimer to rule out PE in pregnancy (overall very poor sensitivity in retrospective analysis)
- In evaluating these patients if there are LE symptoms you should start with a LE doppler
- Currently at BMC VQ scans can be done from 9a-430p
- STAT VQ scans will trigger the tech on call
- CTPA vs VQ scan
- CTPA has much higher radiation to the mother and is more sensitive for detecting PE
- VQ with 10x more radiation to baby due to radionuclide tracer, cannot detect other high risk thoracic pathology, and will likely be abnormal in a patient with underlying lung pathology due to baseline vent/perfusion mismatch
- There are no absolute contraindications for TPA in pregnancy
- In the same vein, no contraindications for ECMO
- Dissection, like in other patients, will present atypically
- SCAD (spontaneous coronary artery dissection)
- Leading cause of mI in pregnancy and postpartum period (majority 3rd trimester)
- Standard of diagnosis is coronary CT or cath
- Treat with antiplatelet, consider AC but not necessary
- ASA is more safe in third trimester
- DAPT can be given
- Beta blockers are category B
- No definitive management options, supportive care and medical management
- Resources
- REBEL EM SCAD
- YEARS criteria for PE in pregnancy
Chest Pain, Pregnancy, and ECMO– Dr Alina Khurgel
- Cardiac arrest in pregnant patients
- Most common: hemorrhage, CHF, pulmonary/amniotic fluid emboli, infection
- BE AWARE that there is significantly higher difference maternal mortality in non-white patients
- Special considerations: continuous lateral uterine displacement (do not put downward pressure), no evidence for Lucas devices
- Prepare for emergency cesarean delivery within 4 minutes
- Video below
- In patients with VT/VF arrest should have high clinical suspicion for ischemia
- If a high suspicion for PE, TPA should be given in the peri-arrest/arrest patient
- Peripartum intubation
- Commonly difficult airways due to airway edema and distortion of anatomy
- Increased risk of hypoxia due to physiologic hyperventilation
- Should avoid nasal airway adjuncts due to friability of upper airway
- ECMO and ECPR considerations
- Young patients (<65), minimal comorbidities, witnessed arrest, >10min of conventional CPR, potential for cardiac recovery, and initiation within 60min
- Institution of VA ECMO during resuscitation
- General indications: cardiac/respiratory failure or combination
- VA- cardiopulmonary bypass
- VV- pulmonary bypass
- BMC indications
- VV ECMO- severe ARDS, asthma, airway obstruction, smoke inhalation
- VA ECMO- heart failure/cardiogenic shock, massive PE, environmental hypothermia
- Resources
- SALAD Technique for airway contamination
- Journal of Intensive Care Medicine ECMO Summary
- EMCRIT Who to refer for VV ECMO
- LITFL ECMO Overview
- Resuscitative hysterotomy simulation
Black History and Medicine– Dr Jaionn Griner
- Brief timeline of significant events in black history
- Juneteenth originated in June 19, 1865 after the emancipation of slaves in Galveston Texas by union troops
- 1896- institution of separate but equal clause in case of Plessy v Ferguson
- 1964- institution of the civil rights act prohibiting discrimination based on race, color, sex, religion, or nationality
- 1966- formation of the black panthers in response to persistent racial inequality and over policing of blacks
- In 1967 in response to police patrols a bill was introduced to repeal open carry of weapons which eventually passed
- 2023- affirmative action deemed unconstitutional by supreme court
- Dark history of medicine
- Tuskegee syphilis study- 40 year study where 400 black men were provided free healthcare in exchange for observation of the disease progression of syphilis
- Ultimately they were lied to about the diagnosis and not treated when the diagnosis was discovered
- Participants expired and had many complications related to the disease
- J. Marion Sims- developed various surgical techniques for OBGYN by operating on enslaved women WITHOUT anesthesia
- During COVID19 pandemic there was a disproportionate amount of black patients who were both infected and died in comparison to white counterparts
- Tuskegee syphilis study- 40 year study where 400 black men were provided free healthcare in exchange for observation of the disease progression of syphilis
- How does this affect us?
- Microaggressions– subtle intentional and unintentional interactions communicating bias towards underrepresented groups
- Microassault- says something discriminatory but does not think their actions are harmful
- Microinsult- unintentional comments said in a discriminatory way
- Microinvalidation- actions and behaviors that deny racism and discrimination
- Stereotype threat– the risk of confirming negative stereotypes about an individual’s identity leading to increased cognitive load
- White supremacy culture– the ideas, beliefs, and actions of white people are superior to people of color
- Reproduced by all institutions in our society to market a white image
- Microaggressions– subtle intentional and unintentional interactions communicating bias towards underrepresented groups
- Resources
- Responsibility of EM providers in anti-racist efforts
- Beyond the scenes: Daily Show “How Racist is Boston”
- How to be Anti-Racist- Ibram Kendi
- Implicit bias testing


Leave a comment